|
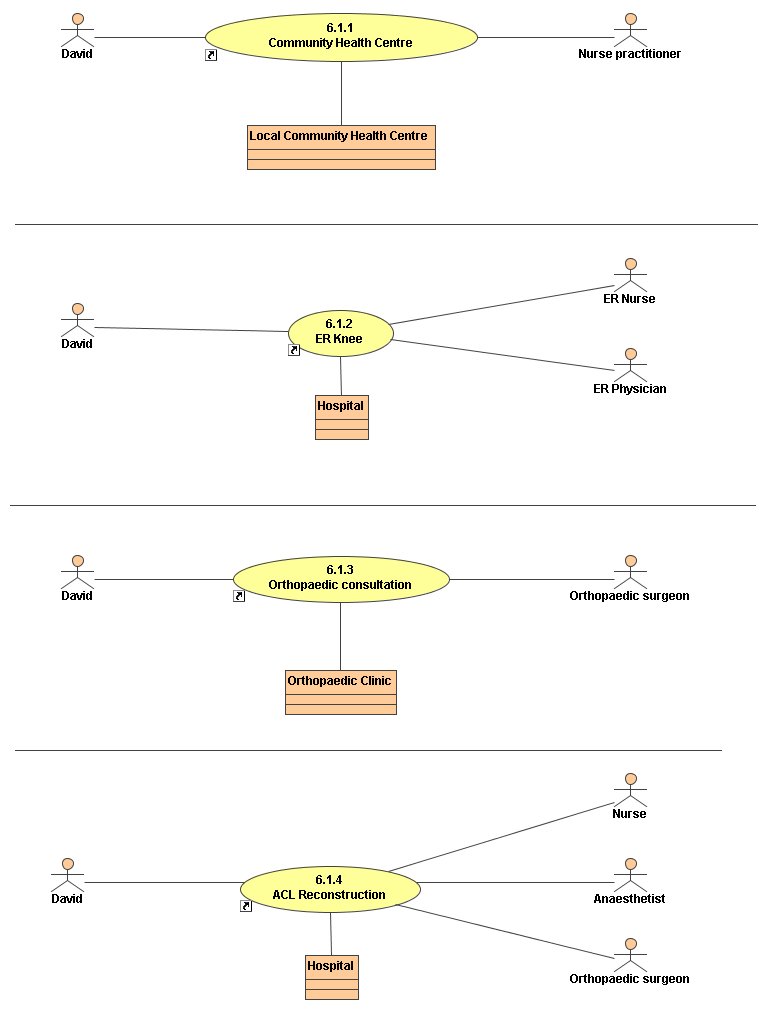
Dr. David Lambert, 40, suffers a significant pivot-type injury to his right knee while on a vacation in one of the territories. He takes an anti-inflammatory medication and develops a rash. The next day he is taken by his companions to the local community health centre for assessment by the nurse practitioner there. She feels he has had a significant knee injury along with an allergic reaction to the medication and that he should be assessed at the nearest hospital.
Later that day David is driven by his friends to the hospital where he is admitted to the ER. The ER physician that evening, a local family physician, takes the history of the injury and examines the knee. An x-ray is taken and does not show a fracture. The physician’s diagnosis is complete anterior cruciate ligament (ACL) tear of the right knee. Crutches, brace and an analgesic are provided and David is discharged from the ER.
David returns home and sees one of the other family doctors in his office, who refers him to an orthopaedic surgeon. The partner creates a consultation request document for the surgeon outlining the history of present illness. This document is sent to the consultant’s office staff who later respond by phone with a place, date and time for the appointment.
The consultation takes place four weeks later at the tertiary care hospital outpatient orthopaedic clinic. The orthopaedic surgeon, Dr. Abram, assesses David’s knee and diagnoses a complete ACL tear with possible medial meniscus tear. He is able to review the x-ray image that was done in the ER shortly after the injury and chooses not to do another. David is referred to a physiotherapist for rehabilitation of the knee.
David attends a local community physiotherapy clinic near his office and works with the physiotherapist over two months but continues to have diffuse pain with occasional locking and instability. The therapist is concerned about the lack of progress and suggests follow up with Dr. Abram.
David returns to see the surgeon at the hospital outpatient orthopaedic clinic. Dr. Abram reviews the history and repeats the physical exam. He is concerned about the limited progress and persistent clinical findings. He orders an MRI to look for meniscus damage and completes the appropriate requisition form, which is then sent to the DI department.
The MRI is done at the hospital 3 months later and shows a substantial medial meniscus tear as well as a complete tear of the ACL. David sees the orthopaedic surgeon again for the results and the decision is made to reconstruct the ACL and address the torn meniscus.
Six weeks later the surgery is done on an outpatient basis and David is discharged home that day with his brace and crutches. His wife, Linda, picks up the prescription for his analgesic medications from a community pharmacy.
Post-operative assessment is done two weeks later at the orthopaedic outpatient clinic at the hospital and progress is good. The orthopaedic surgeon refers David back to physiotherapy to start his rehab.
| General Info | |
|---|---|
| Name | 6.1 ACL Injury Storyboard Diagram |
| Type | Use Case Diagram |